Infectious Diseases pose a significant threat to public health, both in healthcare settings and the wider community. Understanding how germs spread and cause illness is vital in implementing effective infectious disease control measures and minimizing the risk of infection.
Key Takeaways:
- Practicing good hygiene, such as regular hand-washing and covering coughs and sneezes, is essential for preventing the spread of infections.
- Avoiding close contact with sick individuals helps reduce the risk of infection transmission.
- Proper cleaning and disinfection of frequently-touched surfaces play a crucial role in controlling the spread of germs.
- Seeking medical care when experiencing signs and symptoms of infection is essential for timely diagnosis and treatment.
- Vaccination is a vital prevention strategy, protecting individuals and communities from specific diseases.
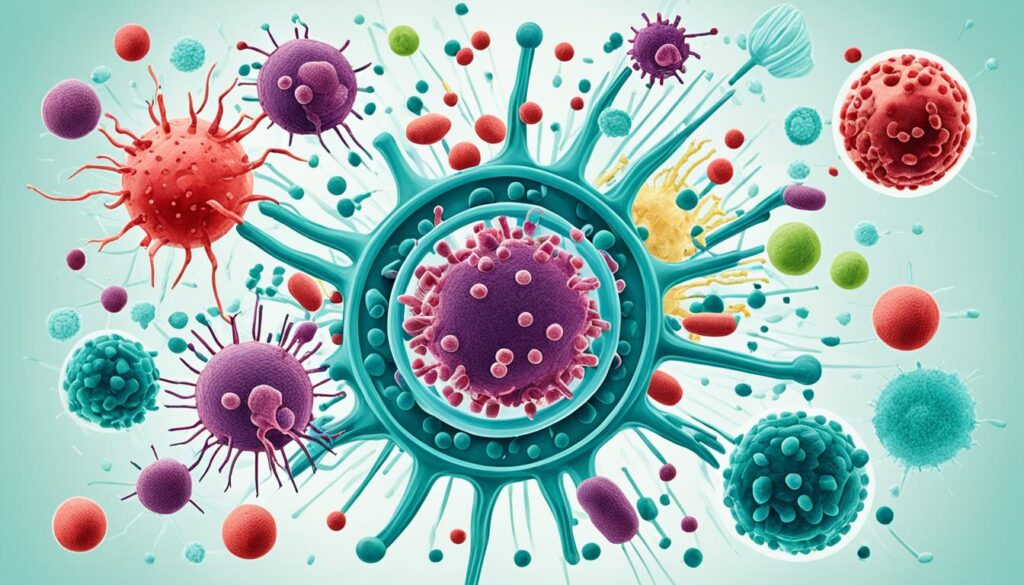
Types of Germs: Bacteria, Viruses, Fungi, Protozoans, and Helminths
Germs come in various forms, including bacteria, viruses, fungi, protozoans, and helminths. Each type of germ has its own characteristics and potential for causing illness.
Bacteria are single-celled organisms that can be both helpful and harmful. While some bacteria are beneficial for digestion and the environment, others can cause infections and diseases. Common bacterial infections include strep throat, tuberculosis, and urinary tract infections.
Viruses are smaller than cells and cannot reproduce on their own. They rely on host cells to replicate and cause infections. Viral infections are prevalent and can range from mild illnesses like the common cold and influenza to severe diseases like COVID-19.
Fungi include organisms like candida and molds. While some fungi are harmless, others can cause infections. Fungal infections can affect various parts of the body and lead to conditions like thrush, athlete’s foot, or even systemic fungal infections in immunocompromised individuals.
Protozoans are single-celled organisms that can cause infections in humans. These parasites can enter the body through contaminated food, water, or insect bites. Examples of diseases caused by protozoans include giardiasis, malaria, and amoebic dysentery.
Helminths are larger parasites, commonly known as worms. They can infect humans and live in various body parts such as the intestines, lungs, liver, skin, or even the brain. Helminthic infections, like tapeworm infestations or roundworm infections, can lead to significant health issues by feeding off the body’s nutrients.
| Type of Germs | Examples |
|---|---|
| Bacteria | Strep throat, tuberculosis, urinary tract infections |
| Viruses | Common cold, influenza, COVID-19 |
| Fungi | Thrush, athlete’s foot |
| Protozoans | Giardiasis, malaria, amoebic dysentery |
| Helminths | Tapeworms, roundworms |
Understanding the different types of germs is crucial for implementing effective prevention and control measures to minimize the risk of infections and diseases. By adopting proper hygiene practices, seeking medical care when necessary, and following recommended vaccination schedules, individuals can protect themselves and contribute to the overall well-being of their communities.
Infection Vs. Disease: Understanding the Difference
When it comes to germs and their impact on our health, it’s essential to understand the difference between infection and disease. While these terms are often used interchangeably, they have distinct meanings.
Infection occurs when germs, such as bacteria or viruses, enter the body and begin to multiply. This can happen through various routes, including inhalation, ingestion, or direct contact with infected individuals or surfaces. However, it’s important to note that not all infections result in illness.
Disease, on the other hand, refers to the actual manifestation of illness that occurs as a result of an infection. Infection becomes a disease when the invading germs damage cells and tissues, leading to signs and symptoms that affect the body’s normal functioning.
Infections can range from mild to severe, and their progression to disease depends on various factors, including the virulence of the germ, the individual’s immune response, and other underlying health conditions. While some infections may go unnoticed or cause minimal symptoms, others can result in serious complications and even be life-threatening.
The immune system plays a crucial role in fighting off infections and preventing them from progressing to disease. It serves as our body’s defense mechanism, identifying and eliminating invading germs to keep us healthy. However, in certain cases, the immune response may be compromised, making individuals more susceptible to infections and increasing the risk of developing diseases.
Recognizing the signs of infection is vital for timely medical intervention and effective disease management. Common signs of infection include fever, fatigue, body aches, cough, sore throat, and gastrointestinal symptoms. If you experience any concerning symptoms or suspect an infection, it’s crucial to seek medical care to receive proper diagnosis, treatment, and preventive measures.
The Importance of Early Detection and Treatment
Early detection and prompt treatment of infections can significantly minimize their impact and prevent the progression to severe diseases. Your healthcare provider can conduct diagnostic tests, identify the specific pathogen causing the infection, and recommend appropriate treatment modalities, including medication, rest, and self-care measures.
Managing infections and preventing them from spreading within communities and healthcare settings are crucial steps in controlling the burden of infectious diseases. By understanding the distinction between infection and disease and taking proactive measures, we can protect ourselves and others from the harmful effects of germs.
Preventing the Spread of Germs: Good Hygiene Practices
Practicing good hygiene is crucial for preventing the spread of germs and infections. By implementing simple yet effective tactics, individuals can significantly reduce the transmission of infectious diseases. Below are some key practices to follow:
- Regular hand-washing: The act of washing hands with soap and water for at least 20 seconds is one of the most effective ways to prevent the spread of germs. This practice should be done thoroughly and regularly, especially before meals, after using the restroom, and when returning home from public spaces.
- Proper cough and sneeze etiquette: When coughing or sneezing, it is essential to cover the mouth and nose with a tissue or the elbow. This practice helps prevent respiratory droplets from being released into the air and spreading germs to others.
- Avoiding face-touching: Touching the face, particularly the eyes, nose, and mouth, can introduce germs from the hands into the body. It is crucial to refrain from unnecessary face-touching to minimize the risk of infection.
- Staying home when sick: If feeling unwell, individuals should avoid going to work, school, or public places to prevent the spread of germs to others. It is important to prioritize rest and recovery while avoiding contact with individuals who may be more vulnerable to infections.
- Cleaning and disinfecting frequently-touched surfaces: Surfaces that are frequently touched, such as doorknobs, light switches, and countertops, can harbor germs. Regularly cleaning and disinfecting these surfaces using appropriate products can help eliminate germs and reduce the risk of infection.
Vaccines also play a crucial role in preventing the spread of certain diseases and protecting public health. By getting vaccinated according to the recommended schedules, individuals contribute to their own well-being and the well-being of the community by reducing the overall prevalence of infectious diseases.
“Practicing good hygiene is not only a personal responsibility but also a collective effort to prevent the spread of germs and protect public health.” – Dr. Amanda Johnson
By incorporating these good hygiene practices into daily routines, individuals can effectively contribute to preventing the spread of germs and infectious diseases. These practices are particularly crucial during outbreaks or when in close proximity to vulnerable populations, such as healthcare settings or crowded environments.
| Hygiene Practice | Benefits |
|---|---|
| Regular hand-washing | – Reduces the risk of contracting and spreading infections – Removes germs from hands |
| Proper cough and sneeze etiquette | – Prevents the release of respiratory droplets containing germs into the air – Minimizes the risk of infecting others |
| Avoiding face-touching | – Reduces the chance of introducing germs from hands into the body – Minimizes the risk of infection |
| Staying home when sick | – Prevents the spread of germs to others – Allows for rest and recovery |
| Cleaning and disinfecting frequently-touched surfaces | – Eliminates germs from surfaces – Reduces the risk of contamination |
When to Seek Medical Care for Infections
Infections can range from mild to severe and may require medical attention depending on the signs and symptoms you experience. It’s important to be aware of certain red flags that indicate the need to seek immediate medical care. If you notice any of the following signs and symptoms, it’s crucial to consult a healthcare provider:
- Difficulty breathing: If you experience shortness of breath, wheezing, or any other breathing difficulties, it may indicate a severe infection that requires urgent medical attention.
- Persistent cough: A cough that persists for an extended period, especially when accompanied by other concerning symptoms, could indicate a respiratory infection that needs medical evaluation.
- Rapid heartbeat: Abnormally fast heart rate, palpitations, or chest pain could be signs of a systemic infection that requires immediate medical care.
- Rash accompanied by fever: If you develop a rash accompanied by a fever, it may indicate an infection, such as an allergic reaction or a viral or bacterial infection.
- Swelling: Sudden and significant swelling, particularly in the throat, face, or extremities, is a cause for concern and should be evaluated by a healthcare professional.
- Blurred vision: Blurred vision, vision loss, or other visual disturbances may be signs of an underlying infection that requires immediate medical attention to prevent complications.
- Vomiting: Repeated episodes of vomiting could be a sign of a severe infection, such as a gastrointestinal infection or food poisoning, that requires medical evaluation.
- Severe headache: Intense, debilitating headaches, especially when accompanied by other symptoms like fever or neck stiffness, should be evaluated by a healthcare provider.
If you experience any of these signs and symptoms, it’s important not to delay seeking medical care. Healthcare providers can conduct diagnostic tests, assess the severity of the infection, and prescribe appropriate treatment to help manage and control infectious diseases.

| Signs and Symptoms | When to Seek Medical Care |
|---|---|
| Difficulty breathing | Immediately |
| Persistent cough | If it lasts for an extended period |
| Rapid heartbeat | If accompanied by other concerning symptoms |
| Rash accompanied by fever | When a rash appears with a fever |
| Swelling | Sudden and significant swelling |
| Blurred vision | When vision becomes blurred or impaired |
| Vomiting | If experiencing repeated episodes of vomiting |
| Severe headache | When the headache is intense and debilitating |
Understanding the Lifespan of Germs on Surfaces
Germs can survive on surfaces for varying periods, depending on factors such as the type of germ, the amount present, the surface material, and environmental conditions. This knowledge is essential in understanding the risk of transmission and implementing effective cleaning and disinfection strategies to minimize the spread of infectious diseases.
Viruses, including those responsible for the common cold and influenza, can live on surfaces for up to 24 to 48 hours. This means that if an infected person touches a surface, such as a doorknob or countertop, the virus can remain viable and potentially infect others who come into contact with the contaminated surface.
Bacteria, such as E. coli, have a shorter lifespan on surfaces compared to viruses. They can survive for up to four hours, making it important to clean and disinfect frequently-touched surfaces regularly to prevent bacterial contamination.
Also Read:- Defend Your Skin: Proven Strategies For Preventing Skin
It’s worth noting that the lifespan of germs on surfaces can be influenced by factors such as humidity, temperature, and the presence of organic matter. For example, some viruses may survive longer in low humidity environments, while bacteria can be more resilient in damp conditions.
To minimize the risk of transmission, proper cleaning and disinfection practices are crucial. Cleaning refers to the removal of dirt, germs, and impurities from surfaces, while disinfection involves using chemicals to kill or inactivate germs. By combining both cleaning and disinfection, you can effectively reduce the presence of germs on surfaces and lower the risk of transmission.
| Germ Type | Lifespan on Surfaces |
|---|---|
| Viruses (e.g., common cold, influenza) | Up to 24 to 48 hours |
| Bacteria (e.g., E. coli) | Up to 4 hours |
Remember, regular cleaning and disinfection of frequently-touched surfaces, such as doorknobs, light switches, and countertops, can significantly reduce the risk of transmission. It’s also important to follow proper hand hygiene practices, such as washing hands with soap and water for at least 20 seconds, to further prevent the spread of germs.
What Kills Germs: Effective Disinfection Methods
Germs can be killed or deactivated through various methods. Here are some effective disinfection methods that can help eliminate germs and reduce the risk of infection:
1. Rubbing Alcohol
Rubbing alcohol containing at least 70% isopropyl alcohol is an effective germ-killing agent. It can be used to disinfect surfaces and objects that may harbor germs. Simply apply the rubbing alcohol to a clean cloth or cotton ball and wipe down the surfaces. Make sure to follow the instructions and allow sufficient contact time for the alcohol to work its magic.
2. Hydrogen Peroxide
Hydrogen peroxide is another effective disinfectant that can kill a wide range of germs. It can be used to disinfect surfaces, countertops, and even wounds. Apply hydrogen peroxide directly to the area, let it sit for a few minutes, and then wipe it clean. Remember to always check the concentration and follow the instructions for safe use.
3. Hot Water and Soap
For hand hygiene and cleaning surfaces, hot water and soap are highly effective in washing away germs. Washing your hands with soap and water for at least 20 seconds helps remove germs from your skin. Similarly, using hot water and soap to clean surfaces and utensils can eliminate germs and reduce the risk of contamination.
It’s important to note that vinegar is not an effective germ-killing agent and should not be solely relied upon for disinfection. Proper disinfection methods, including the use of appropriate cleaning products, should always be followed to ensure effective germ elimination.
To effectively kill germs and minimize the risk of infection, it’s crucial to implement proper disinfection methods and maintain good hygiene practices. Consistently disinfecting frequently-touched surfaces, practicing regular hand hygiene, and using appropriate disinfectants are key steps in preventing the spread of germs and maintaining a clean and safe environment.

Prevention Beyond Hand-Washing: Additional Strategies
While hand-washing is crucial for preventing the spread of germs, there are other strategies that can further enhance infection control. By implementing these additional prevention strategies, individuals and communities can strengthen their defense against infectious diseases and promote public health.
- Avoiding close contact with sick individuals: Limiting close contact with individuals who are sick can help reduce the risk of contracting and transmitting infectious diseases. Maintaining a safe distance, especially from those displaying symptoms like coughing or sneezing, is crucial.
- Practicing respiratory hygiene: Covering your mouth and nose with a tissue or the inside of your elbow when coughing or sneezing can prevent the spread of respiratory droplets containing germs. Proper disposal of tissues and regular hand-washing afterward is essential.
- Staying home when sick: If you are feeling unwell or experiencing symptoms of an infectious disease, it is important to stay home to prevent the spread of germs to others. This not only protects those around you but also aids in your own recovery.
- Practicing safe food handling: Properly washing fruits and vegetables, cooking foods to appropriate temperatures, and avoiding cross-contamination can minimize the risk of foodborne illnesses caused by harmful bacteria or viruses.
- Maintaining a clean and disinfected environment: Regular cleaning and disinfection of frequently-touched surfaces, such as doorknobs, light switches, and countertops, can help eliminate germs and reduce the risk of transmission between individuals.
Vaccination is also a vital prevention strategy that plays a significant role in infection control. Vaccines are designed to stimulate the immune system and protect against specific diseases. By receiving recommended vaccinations, individuals can develop immunity and contribute to population-level protection.
Implementing these additional prevention strategies, along with practicing good hand hygiene, creates a multi-faceted approach to infection control. By combining these measures, individuals and communities can effectively minimize the risk of infection and promote a healthier environment.

History of Germs: Discovering Microorganisms
The understanding and discovery of germs have significantly evolved over time. Pioneering scientists have made groundbreaking contributions, unraveling the mysteries of microorganisms. In the 17th century, Antonie van Leeuwenhoek’s observation of bacteria through early microscopes laid the foundation for modern microbiology.
“I now observed larger and smaller animals, as to length, move quit freely in the water and I realized that these were living creatures.” – Antonie van Leeuwenhoek
However, it was the advent of Louis Pasteur’s germ theory of disease in the 19th century that revolutionized our understanding of how germs cause infections. Pasteur’s experiments and discoveries were instrumental in establishing the link between microorganisms and diseases, paving the way for significant advancements in infectious disease control and prevention.
“It is within the microbes that Pasteur discovered truths that transformed the future of medicine.” – K.C. Huang
Since Pasteur’s groundbreaking work, the field of microbiology has witnessed continued progress, enabling a deeper understanding of germs and their impact on human health. Ongoing research, technological advancements, and collaborative efforts in the scientific community continue to reveal fascinating insights into microorganisms and their role in infectious diseases.
To gain a better understanding of the development of our knowledge about germs and microorganisms, let’s take a look at the timeline of significant milestones:
| Year | Discovery/Advancement |
|---|---|
| 1674 | Antonie van Leeuwenhoek’s observations of bacteria through microscopes |
| 1861 | First publication of “germ theory” by Louis Pasteur |
| 1882 | Discovery of Mycobacterium tuberculosis by Robert Koch |
| 1928 | Discovery of penicillin by Alexander Fleming |
| 1953 | Discovery of the structure of DNA by James Watson and Francis Crick |
| 1983 | Identification of the human immunodeficiency virus (HIV) |
This timeline highlights key milestones in the history of germs and microorganisms, demonstrating the continuous progress in understanding the microbial world. Through scientific breakthroughs and relentless dedication, researchers have unraveled the complexities of germs, opening avenues for effective infectious disease control, prevention, and treatment.
The Importance of Hygiene and Prevention
Good hygiene practices and prevention strategies are crucial in controlling the spread of infectious diseases. By implementing proper hand hygiene, practicing respiratory etiquette, staying home when sick, and following recommended vaccination schedules, individuals, healthcare settings, and communities can effectively halt the transmission of diseases, protecting public health.
Proper hand hygiene, including regular hand-washing with soap and water for at least 20 seconds, is one of the most essential preventive measures in reducing the risk of infection. It is important to wash hands before and after handling food, before eating, after using the restroom, and after coughing or sneezing to prevent the spread of germs. By incorporating this simple habit into our daily routine, we can significantly reduce the transmission of infectious diseases.
Practicing respiratory etiquette, such as covering coughs and sneezes with a tissue or the inside of the elbow, can prevent the release of respiratory droplets containing infectious germs into the air. This practice is especially important in public settings to protect others from potential exposure.
Staying home when sick is another crucial aspect of infection prevention. By avoiding close contact with others when experiencing symptoms such as fever, cough, or sore throat, the risk of spreading infectious diseases can be minimized. It is important to prioritize personal and public health by seeking medical attention when necessary and following healthcare provider’s advice.
Following recommended vaccination schedules is essential in preventing the occurrence and spread of vaccine-preventable diseases. Vaccines stimulate the immune system to recognize and fight specific infections, helping to develop immunity against diseases such as measles, influenza, and hepatitis. By getting vaccinated and ensuring that immunizations are up-to-date, individuals can protect themselves, their families, and the broader community from infectious diseases.
Overall, prioritizing hygiene and prevention strategies is key to safeguarding individuals and communities from the impact of infectious diseases. By implementing these measures consistently and promoting a culture of infection control, we can create healthier environments and reduce the burden of preventable illnesses.
Comparison of Hygiene Practices and Prevention Strategies
| Hygiene Practices | Prevention Strategies |
|---|---|
| Regular hand-washing | Following recommended vaccination schedules |
| Covering coughs and sneezes | Practicing respiratory etiquette |
| Avoiding close contact when sick | Staying home when experiencing symptoms |
| Cleaning and disinfecting frequently-touched surfaces | Seeking medical care when necessary |
By incorporating these hygiene practices and prevention strategies into our daily lives, we can contribute to a healthier and safer future, protecting ourselves and those around us from infectious diseases.
Conclusion
Preventing and controlling the spread of infectious diseases is crucial for maintaining public health. By understanding the different types of germs, practicing good hygiene, seeking medical care when necessary, and implementing effective prevention strategies, individuals and communities can minimize the risk of infection and reduce the burden of infectious diseases.
Emphasizing the importance of infectious disease control in healthcare settings and beyond is essential for creating a safe and healthy environment for all. By prioritizing infectious disease control measures, such as regular hand-washing, covering coughs and sneezes, and staying home when sick, we can significantly contribute to preventing the transmission of diseases and protecting public health.
Prevention is the key to reducing the impact of infectious diseases on individuals, communities, and the healthcare system as a whole. By promoting good hygiene practices, practicing respiratory etiquette, and ensuring timely access to medical care, we can collectively work towards a healthier and safer future.
FAQs
Q: What is infection control and why is it important?
A: Infection control refers to the practice of preventing infections from spreading. It is crucial in healthcare settings to protect patients, healthcare providers, and visitors from acquiring and transmitting infectious diseases.
Q: How can I get in touch with the bureau of infectious disease prevention and control?
A: You can contact the bureau of infectious disease prevention and control through their official website or by reaching out to your local health department for more information and resources.
Q: What are some infection control practices in healthcare?
A: In healthcare, infection control practices include proper hand hygiene, use of personal protective equipment, environmental cleaning, and adherence to standard precautions to prevent the spread of infectious diseases.
Q: What does the CDC recommend for infection control in healthcare settings?
A: The CDC provides guidelines and recommendations for infection prevention and control in healthcare settings. This includes protocols for surveillance, facility infection control, and disease prevention to ensure patient and healthcare worker safety.
Q: How can healthcare providers ensure infection control in their facilities?
A: Healthcare providers can ensure infection control in their facilities by implementing training programs, updating infection control practices, and collaborating with public health authorities to stay informed about the latest recommendations and requirements.
Q: What role does the Department of Health play in infection prevention and control?
A: The Department of Health plays a key role in providing guidance, assistance, and monitoring of infection prevention and control practices to healthcare facilities, as well as addressing infectious disease outbreaks in collaboration with other organizations.
Q: Why is surveillance important in infection control?
A: Surveillance is crucial in infection control as it helps in the early detection of infectious diseases, monitoring their spread, and implementing appropriate measures to prevent outbreaks and protect public health.
Q: What are some common infection control recommendations for healthcare workers?
A: Some common recommendations for healthcare workers include proper use of personal protective equipment, adherence to standard precautions, and staying updated on infection control guidelines and procedures.
Q: How does the Bureau of Infectious Disease Prevention and Control collaborate with healthcare facilities?
A: The Bureau collaborates with healthcare facilities by providing resources, guidelines, and assistance in implementing infection control practices, as well as conducting investigations and delivering updates on infectious diseases.
Q: What are the minimum requirements for infection control in health facilities?
A: The minimum requirements for infection control in health facilities include the implementation of standard precautions, proper handling and disposal of infectious materials, regular environmental cleaning, and training of healthcare workers in infection control practices.